Trigger for development (1989)
I graduated from Faculty of Medicine, Kagoshima University in 1973 and entered the First Department of Internal Medicine, Kagoshima University Hospital, and engaged in medical practice and research as a clinician specialized in the cardiovascular system. After that, in January 1989, I was transferred from the First Department of Internal Medicine to the Kirishima Rehabilitation Center. Soon after the transfer, I had an encounter at a hospital in Kagoshima City where I engaged in medical practice once a week. A patient who had severe heart failure kept saying to the nurses, “I want to sit in a hot spring once again before I die.” This was a trigger for the development of Waon therapy. Since then I have devoted myself to developing thermal therapy for chronic heart failure patients. The patient was 76 years old, hospitalized for over a year, and at the end-stage heart failure. Kirishima Rehabilitation Center was fully equipped with hot spring facilities, and I always enjoyed the hot spring after conducting medical practice. I recalled the patient every time I bathed in the hot spring and was thinking about whether I could grant the wish of the patient. Bathing is contraindicated for severe heart failure, but no clear reason is found in the literature, so I decided to examine the effect of bathing on the heart. I first decided to examine the effect of bathing on the heart by recording echocardiograms because I was specialized in it. I recorded echocardiograms and expiratory gases during bathing in cooperation with medical student who came for clinical training.
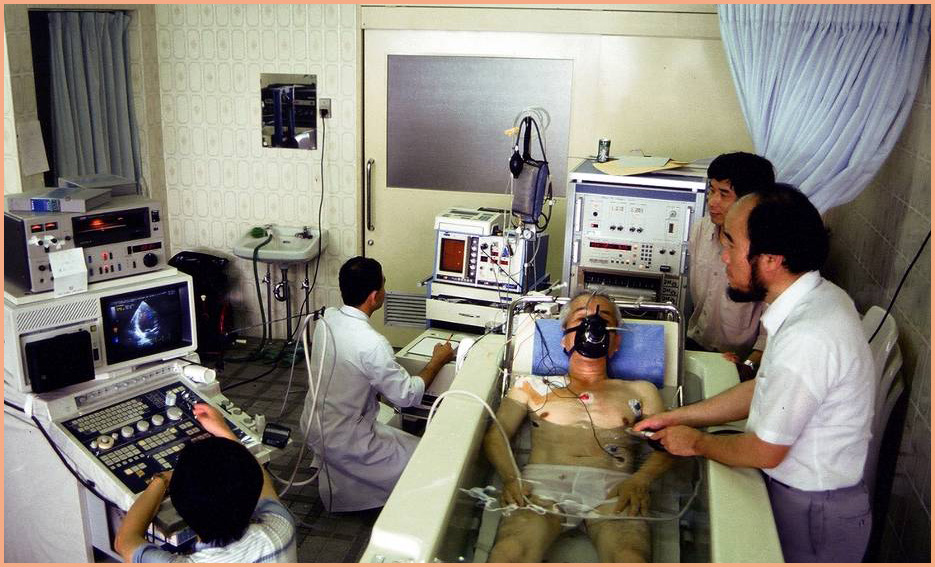
Obtaining echocardiogram and expiratory gas during bathing with the automatic elevating bathtub (1989)
Exercise also increases cardiac output but increases oxygen consumption at the same time. For example, slow walking on an even road is associated with a three- to four-fold increase in oxygen consumption, and exercise is thus restricted in severe heart failure patients. However, oxygen consumption was only slightly increased (0.3- to 0.4-fold) when expiratory gases were measured during bathing with the automatic elevating bathtub because subjects took the bath at rest. In other words, bathing with the automatic elevating bathtub was found to increase cardiac output with only a slight increase in oxygen consumption. Therefore, I thought that bathing with the automatic elevating bathtub was feasible in severe heart failure patients. Blood pressure and heart rate during bathing vary by bathing temperature and time, and I confirmed that the variation in blood pressure and heart rate was acceptable with comfortable bathing temperature for subjects and with a few minutes of bathing time. I was convinced that I would be able to fulfill the wish of the patient with the automatic elevating bathtub.
Realizing hot spring bathing for a severe heart failure patient (1989)
I obtained consent from the patient and the family, took the ambulance with the patient, and transferred the patient to Kirishima Rehabilitation Center. On the next day, I filled the automatic elevating bathtub with Kirishima Hot Spring water, elevated the bathtub while paying attention to the water temperature, and completely immersed the patient in Kirishima Hot Spring water at a comfortable temperature for the patient. Then, the patient slowly took a large deep breath. For a moment, in a cold sweat, I thought he was dying, and held the defibrillator hard, but no change was observed in the rhythm on the ECG monitoring. When I quickly looked at the patient, who was calling me “doctor,” the patient joined his hands in prayer with his eyes full of tears and said, “I can die happy now.” This scene is burned into my memory. Bathing the patient in a hot spring with the automatic elevating bathtub became my routine from the next day because the patient was very satisfied and grateful. Then, surprisingly, week by week the patient recovered, beyond recognition, and was discharged and walked home two months later.
Measuring hemodynamics of heart failure patients during bathing (1989-1991)
I decided to examine the change in hemodynamics by bathing among heart failure patients because it was confirmed in healthy subjects that oxygen consumption was slightly increased and cardiac output was significantly increased by bathing with the automatic elevating bathtub. I obtained consent from heart failure patients, inserted a Swan-Ganz catheter in the right jugular vein, and then measured intra-cardiac pressures (right atrial pressure, pulmonary artery pressure, and pulmonary capillary wedge pressure) before, during, and after bathing simultaneously with echocardiograms and expiratory gases with the automatic elevating bathtub. As a result, the intra-cardiac pressures were confirmed to be significantly increased during bathing. An increase in intra-cardiac pressures shows the increase in the burden on the heart, which is not preferable for heart failure. However, when the bathtub was lowered and the subjects came out of the bathtub, the intra-cardiac pressures were lower than before bathing, indicating that the burden on the heart was decreased. These facts showed that intra-cardiac pressures were increased by increased venous flow by hydrostatic pressure during bathing, but the effect of hydrostatic pressure disappeared after getting out of the bathtub, and showed that the increase in body temperature by bathing dilated the arteries and veins and reduced cardiac preload and afterload. Reduction of cardiac preload and afterload is preferable for heart failure, but increases in oxygen consumption and intra-cardiac pressures are unavoidable with normal bathing or immersion in a hot spring. It was identified again that severe heart failure patients needed to bathe carefully or attentively.
Simultaneously measuring echocardiograms, expiratory gases, and intra-cardiac pressures while in the far-infrared-ray dry sauna room among heart failure patients (1990-1992)
The far-infrared-ray dry sauna room was developed for clinical trials where echocardiograms, expiratory gases, and intra-cardiac pressures were simultaneously recorded. In this sauna room, a portable bed was placed near the wall of the room. A hole to record echocardiograms, electrocardiograms, and blood pressure was made along the side, and a window for measuring the intra-cardiac pressures and expiratory gas were created near the head. After the Swan-Ganz catheter was inserted in the right jugular vein, patients were laid on the bed in a supine position in the sauna room. Echocardiograms, expiratory gases, and intra-cardiac pressures during the sauna were simultaneously recorded, and those before, during, and after the sauna were compared. During the sauna, oxygen consumption was minor, the cardiac output was increased, and intra-cardiac pressures were decreased. The decrease in the intra-cardiac pressure during sauna was the opposite of the increase in the intra-cardiac pressures during bathing with the automatic elevating bathtub.
Changes in hemodynamics were different by the temperature of the dry sauna room, time in the sauna room, time for rest with sufficient warmth after the sauna, etc. Eventually, thermal therapy was determined to be prescribed for heart failure as a 15-minute dry sauna maintained at 60°C at the height of the bed and a bed to rest with sufficient warmth for an additional 30 minutes. An increase in deep-body temperature of about 1.0°C was confirmed at this time by measurement of temperature by the Swan-Ganz catheter in the pulmonary artery.

Verifying the efficacy of thermal therapy in chronic heart failure (1993-1997)
The therapeutic effect of far-infrared-ray dry sauna once daily for four weeks was revealed in patients in whom chronic heart failure is poorly controlled by medication. However, it was premature for general cardiovascular specialists to accept the effect of thermal therapy for chronic heart failure. I decided to review the efficacy of thermal therapy on heart failure at the Mayo Clinic, which is considered a worldwide mecca of clinical medicine, and went to study abroad at the Mayo Clinic from 1994 to 1996. More than one year was required to obtain approval for the clinical research protocol from the institutional review board (IRB), and 1.5 years was required to open the sauna treatment room. We suffered from subject enrollment because of the strict protocol, but managed to finish the clinical trial and confirmed the safety and efficacy of dry sauna treatment for heart failure at the Mayo Clinic as well.
In 1995, clinical research on hemodynamic changes by the automatic elevating bathtub and far-infrared-ray dry sauna among chronic heart failure patients that was conducted at the Kirishima Rehabilitation Center appeared in ‘Circulation’, a prestigious journal in cardiovascular medicine.
Various effects of treatment of chronic heart failure with far-infrared-ray dry sauna:
Clinical research and confirmation by experiments with small animals (1998-2006)
In April 1998 I returned to my former workplace, the First Department of Internal Medicine, Kagoshima University Faculty of Medicine as a professor and chief from the Kirishima Rehabilitation Center. As a result, with an increase in staff, I started clinical research to confirm the efficacy of thermal therapy in various intractable diseases in addition to chronic heart failure. I also confirmed the efficacy identified in clinical settings and uncovered the mechanism of the effect using small animals such as hamsters and mice.
In clinical research for chronic heart failure, the improvement of vascular endothelial functions in heart failure patients, improvement of arrhythmia, and improvement of vascular endothelial functions in lifestyle-related diseases with risk factors were revealed. Clinical research for arteriosclerosis obliterans showed pain relief, improvement of walking distance, and marked improvement in severe lower-limb ischemia patients in which lower limb amputation was indicated.
In other clinical research, thermal therapy was confirmed to be effective for intractable chronic fatigue syndrome, persistent fibromyalgia syndrome, poor salivation, recurred postoperative ileus, etc.
In basic research using small animals, thermal therapy was proved to improve the prognosis of all heart failure model hamsters, increase gene expression of NO synthetase, and enhance the expression of NO protein.
Changing the name from “thermal therapy” to “Waon therapy” (2007)
Subsequent clinical research and basic research (2007-2012)
We thought that the name of our thermal therapy, in which the entire body is comfortably warmed, needed to be changed in order to differentiate it from local high heat therapy for cancer. In March 2007 I changed the name from “thermal therapy” to “Waon therapy.” Waon literally means “soothing warm.” Waon therapy or soothing warm therapy is extremely safe and is a kind comprehensive treatment method for patients because of its soothing power and the fact that it prompts a refreshing positive perspiration. The word Waon is a term that I coined, and it is used in the English translation as it is pronounced in Japanese. Today, Waon therapy is known both domestically and abroad. The article entitled “Waon Therapy Improves Peripheral Arterial Disease.” was published in J Am Coll Cardiol 2007; 50: 2169-2172. In 2011 the European Heart Journal introduced “Waon therapy” as a new therapy for intractable heart failure.
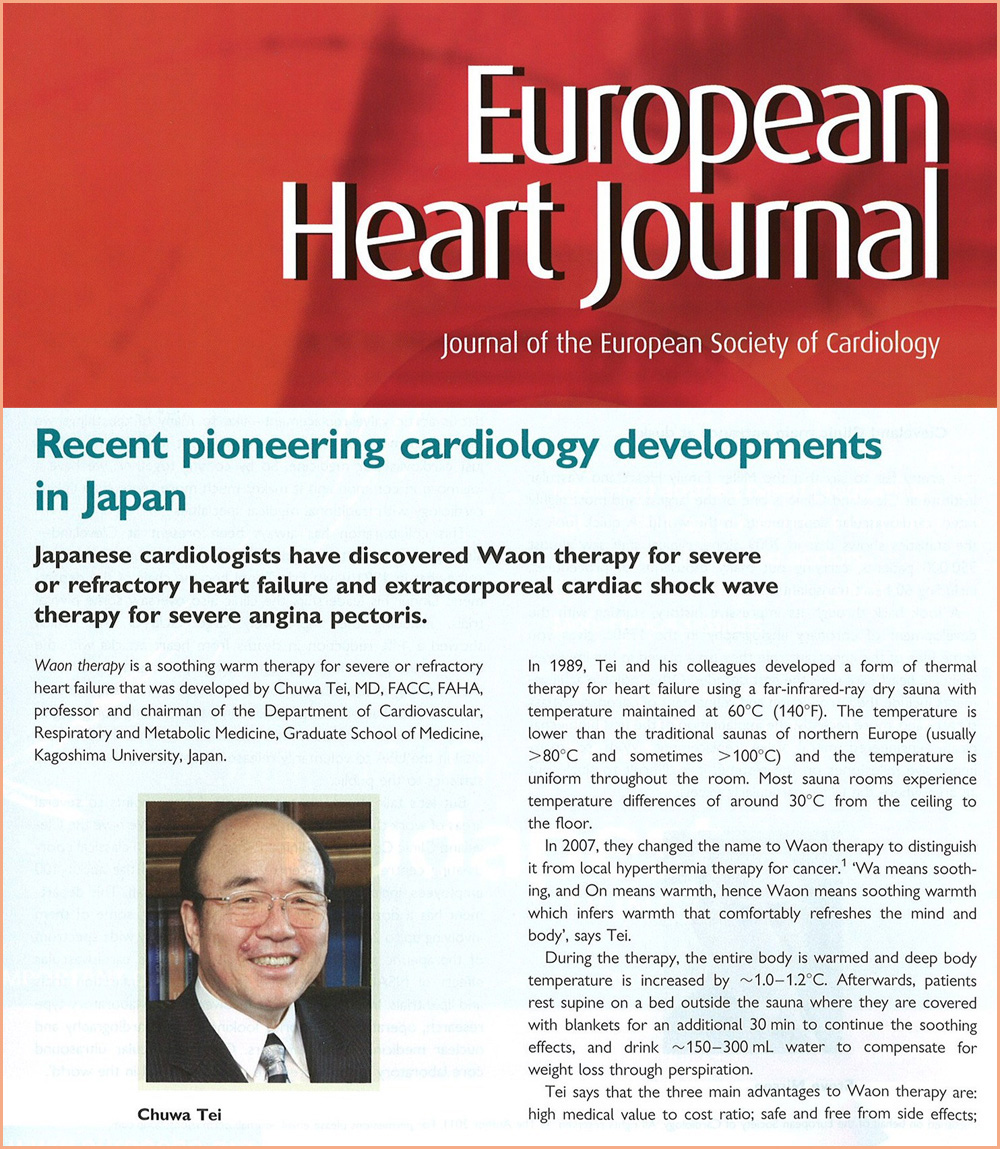 In 2008 a multicenter prospective comparative clinical trial in 10 cardiovascular facilities in Japan was conducted in 188 chronic heart failure subjects to confirm the safety and usefulness of Waon therapy. In the Waon therapy group that received Waon therapy once daily, the clinical symptoms of heart failure and cardiac functions were significantly improved, which confirmed that Waon therapy was a safe and effective therapy to reduce heart enlargement.
In 2008 a multicenter prospective comparative clinical trial in 10 cardiovascular facilities in Japan was conducted in 188 chronic heart failure subjects to confirm the safety and usefulness of Waon therapy. In the Waon therapy group that received Waon therapy once daily, the clinical symptoms of heart failure and cardiac functions were significantly improved, which confirmed that Waon therapy was a safe and effective therapy to reduce heart enlargement.
In 2009 the medication group and medication + twice-weekly Waon therapy group were observed for five years in a retrospective study of 120 chronic heart failure patients. As a result, the mortality rate and readmission rate due to heart failure during the follow-up period were significantly decreased with Waon therapy. In the same year, Mayo Clinic also reported that Waon therapy in chronic heart failure patients was a safe therapy without adverse reactions.
In the 2010 revised issue of the Japanese Circulation Society Guidelines (Guidelines for Treatment of Chronic Heart Failure [JCS 2010]), Waon therapy was listed as a Class I treatment, meaning it is "useful and effective" for chronic heart failure, and was approved as a recommended therapy among cardiovascular specialists.
![Guidelines for Treatment of Chronic Heart Failure [JCS 2010]](../img/08_image0803.jpg) In September 2011 Waon therapy was recognized as a highly advanced medical treatment for chronic heart failure at a specialized conference in this field.
In September 2011 Waon therapy was recognized as a highly advanced medical treatment for chronic heart failure at a specialized conference in this field.
At the biennial reviews of Japan's National Health Insurance coverage in 2012 and 2014, the Japanese Circulation Society, Japanese College of Cardiology, and the Japanese Heart Failure Society recommended Waon therapy for chronic heart failure as the first rank for National Health Insurance coverage. This recommendation for Waon therapy by these three prestigious societies proves that the safety and usefulness of Waon therapy was approved by specialized medical societies. However, Waon therapy was not approved for the National Health Insurance coverage because of flawed paperwork; there was a description in the package insert of “Waon Equipment”: “It is contraindicated for heart failure.”
May 2012 to present (November 2014)
I set up the Waon Therapy Research Institute in May 2012 in order to establish and popularize Waon therapy. To delete the contraindications written in the "Waon Equipment" package insert, a prospective multicenter randomized comparative clinical study of Waon therapy was started from 2012 in guidance and cooperation of University of Tokyo Translational Research Center. The enrollment of 152 severe heart failure subjects in this prospective multicenter randomized comparative clinical study, in which 19 institutions, including 16 university hospitals nationwide, participated, was completed at the end of April 2014. No adverse event that was directly related to Waon therapy was found in this prospective multicenter clinical study, and the issue of the package insert was resolved in October 2014 after reconfirming safety.
Waon therapy appeared in the Journal of JCS Cardiologists (vol. 22, no. 1) in March 2014 as "a therapy developed in Japan," and it can be seen that Waon therapy is recognized as "safe and effective therapy for heart failure" by cardiologists. It is expected to help many heart failure patients by being covered by National Health Insurance.
Future development and final goals (2015 and beyond)
We will realize the coverage of Waon therapy for chronic cardiac failure by National Health Insurance, and we will also conduct clinical trials of Waon therapy for severe lower-limb ischemia and aim for the coverage of this indication by National Health Insurance. In addition, we will compile evidence to confirm the efficacy of Waon therapy in other intractable diseases and aim at providing good news for patients with various intractable diseases.
The final goals of Waon therapy are:
1) To promote a happy long life in our long-lived society as holistic medical care, and
2) To realize a happy long life in which a person can experience the period of receiving nursing care in happiness.
We aim to establish Waon therapy as medical care for the elderly all over the world to live with happiness beyond categories of gender and race.